Beyond the Antacid: Why Your Reflux Might Be a Gut Problem (Not Just an Acid Problem)
You've been told it's "just acid reflux." Pop a Mylanta, take your PPI, avoid spicy foods. But what if I told you that up to 50% of people with GORD get minimal relief from acid suppression medication?
As a naturopath who specialises in gut health, I see this constantly. Clients come to me after years on PPIs, still suffering, still searching for answers. And here's what the research is finally catching up to: GORD isn't just about excess acid—it's also about your microbiome.
The Changing Face of Reflux
GORD used to be considered a "middle-aged disease." Not anymore. The biggest increase in prevalence is now in 30-39 year-olds, driven by obesity rates and poor dietary habits. If you're young and struggling with reflux, you're not alone—and you deserve better answers than "take this pill forever."
What's Really Going On?
Here's what we now know: The refluxate (the stuff that comes back up) isn't just acid. It's a toxic cocktail of:
Pepsin
Bile acids
Gut bacteria (yes, bacteria!)
Gastric acid
Each of these components triggers inflammation and damages your oesophageal tissue in different ways. This is why blocking acid alone doesn't work for everyone.
The Microbiome Connection: The Missing Link
Your oesophagus (the tube connecting your mouth to your stomach) has its own community of bacteria, different from what lives in your mouth or stomach. In healthy people, it's home to beneficial "friendly" bacteria.
But in people with GORD? The neighborhood changes.
The wrong types of bacteria move in and take over. These troublemaker bacteria release toxic substances that set off a chain reaction of inflammation.
This inflammation:
Damages the protective lining of your oesophagus
Leaves nerve endings exposed and raw (hello, pain!)
Weakens the valve that's supposed to keep stomach acid down
Slows down how quickly your stomach empties
In other words: When the bacterial balance in your oesophagus goes wrong (dysbiosis), it creates the perfect conditions for reflux to happen and keep happening.
This is why simply blocking acid often doesn't fix the problem—you need to fix the bacterial imbalance that's causing all this chaos in the first place.
The PPI Paradox: When the Cure Makes It Worse
Here's the kicker that drives me absolutely crazy: The standard treatment for GORD—proton pump inhibitors—actually makes your microbiome worse.
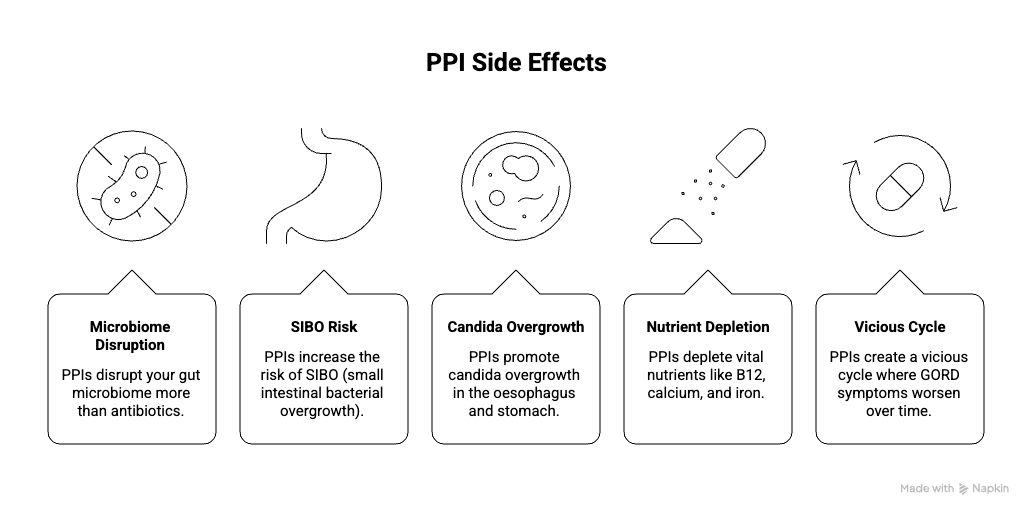
Research shows PPIs:
So you take PPIs to reduce acid, which worsens your dysbiosis, which worsens your GORD. See the problem?
The SIBO-GORD Connection
Speaking of SIBO—there's a strong correlation between SIBO and GORD. When bacteria overgrow in your small intestine, they produce excess gas. This increases abdominal pressure, delays transit, increases inflammation, and literally pushes stomach contents back up into your oesophagus.
And guess what promotes SIBO? Long-term PPI use.
Constipation also worsens reflux through the same mechanism—slow transit time and increased pressure.
This is why I always investigate the ENTIRE digestive tract, not just prescribe an antacid.
The Stress Factor: Your Brain-Gut Connection
Your gut and brain are constantly talking to each other, and stress plays a huge role in reflux.
Think of it this way: when you're stressed, your body goes into survival mode. This triggers a domino effect in your digestive system:
What happens when you're stressed:
Your body releases stress hormones
The valve at the top of your stomach (that's supposed to keep food down) relaxes and gets floppy
Your stomach empties slower—food just sits there longer
Your gut becomes more sensitive to pain and discomfort
The result? All the perfect conditions for reflux.
This is why your heartburn flares up when you're anxious, overwhelmed, or going through a stressful period. It's not "all in your head"—it's your brain and gut working together (unfortunately, against you in this case).
The stress isn't causing imaginary symptoms. It's causing real, physical changes in how your digestive system works.
Evidence-Based Natural Approaches
So what actually works? Here's what the research shows:
Probiotics: Targeting the Root Cause
My favourite Lactobacillus strains that shows real promise:
Lactobacillus reuteri DSM 17938 decreased SIBO rates and digestive symptoms in children on PPIs (reducing dysbiosis from 56.2% to just 6.2%!)
Herbal Heroes
Research backs several botanicals for GORD:
Licorice (deglycyrrhizinated)
75mg twice daily significantly improved quality of life
Reduced heartburn and regurgitation frequency
Works through antioxidant, anti-inflammatory, and mucosal restorative actions
Mastic Gum
1000mg three times daily was as effective as omeprazole for symptom relief
Antiulcer, anti-inflammatory, and mucosal protective properties
Aloe Vera
Reduced heartburn and burping at both 2 and 4 weeks
Less effective than PPIs but without the side effects and rebound
Fibre: The Underrated Game-Changer
Psyllium showed remarkable results:
5g three times daily reduced heartburn and reflux episodes
Increased lower oesophageal sphincter pressure
More effective than omeprazole at preventing recurrence (24.2% vs 69.8%)
Better safety profile with no rebound acid production
The fibre works because most people with GORD have inadequate fibre intake (less than 20g daily). Fibre helps with motility, supports beneficial bacteria, and reduces abdominal pressure.
My Detective Approach: Investigating the Real Causes
When someone comes to me with GORD, I don't just mask symptoms. I investigate:
The Bottom Line
GORD is not a life sentence, and PPIs are not your only option.
The emerging research makes it crystal clear: reflux is a microbiome problem as much as (or more than) an acid problem. By addressing dysbiosis, supporting beneficial bacteria, optimising fibre intake, managing stress, and using targeted botanicals, I tackle the root cause—not just suppress symptoms.
If you've been struggling with GORD and conventional treatment isn't cutting it, it's time to look beyond the antacid and investigate what's really going on in your gut.